10 Questions to Ask Your ABA Provider (Even If You Feel Awkward)

A guide for parents who want clarity, dignity, and real progress
Many parents walk into ABA intake meetings already carrying fear — fear that asking too many questions could delay services, push their child further down an already long waitlist, or label them as “difficult” in a system where access feels fragile. So they stay quiet. They nod along, accept vague explanations, and hold their real questions back, telling themselves they’ll speak up later, once services feel secure. More often than not, they leave those meetings with more anxiety than confidence. That silence is understandable — but it should not be required. ABA is healthcare. You are not asking for favors; you are hiring a clinical service for your child. Asking questions does not slow care. It protects it. These questions aren’t about creating conflict or challenging your provider — they’re about understanding who is working with your child, what they’re teaching, how progress is measured, and what happens when something doesn’t feel right. This guide exists to give you the language, confidence, and permission to ask.
The 10 questions you should be asking (but are often afraid to)
1. Who exactly will work with my child, and what are their credentials?
Most direct therapy is delivered by technicians, not the BCBA. That is normal. What matters is that you understand who is doing what.
A strong answer sounds like:
A BCBA designs and oversees the treatment plan
Trained technicians deliver day-to-day therapy
Clear explanation of supervision and training
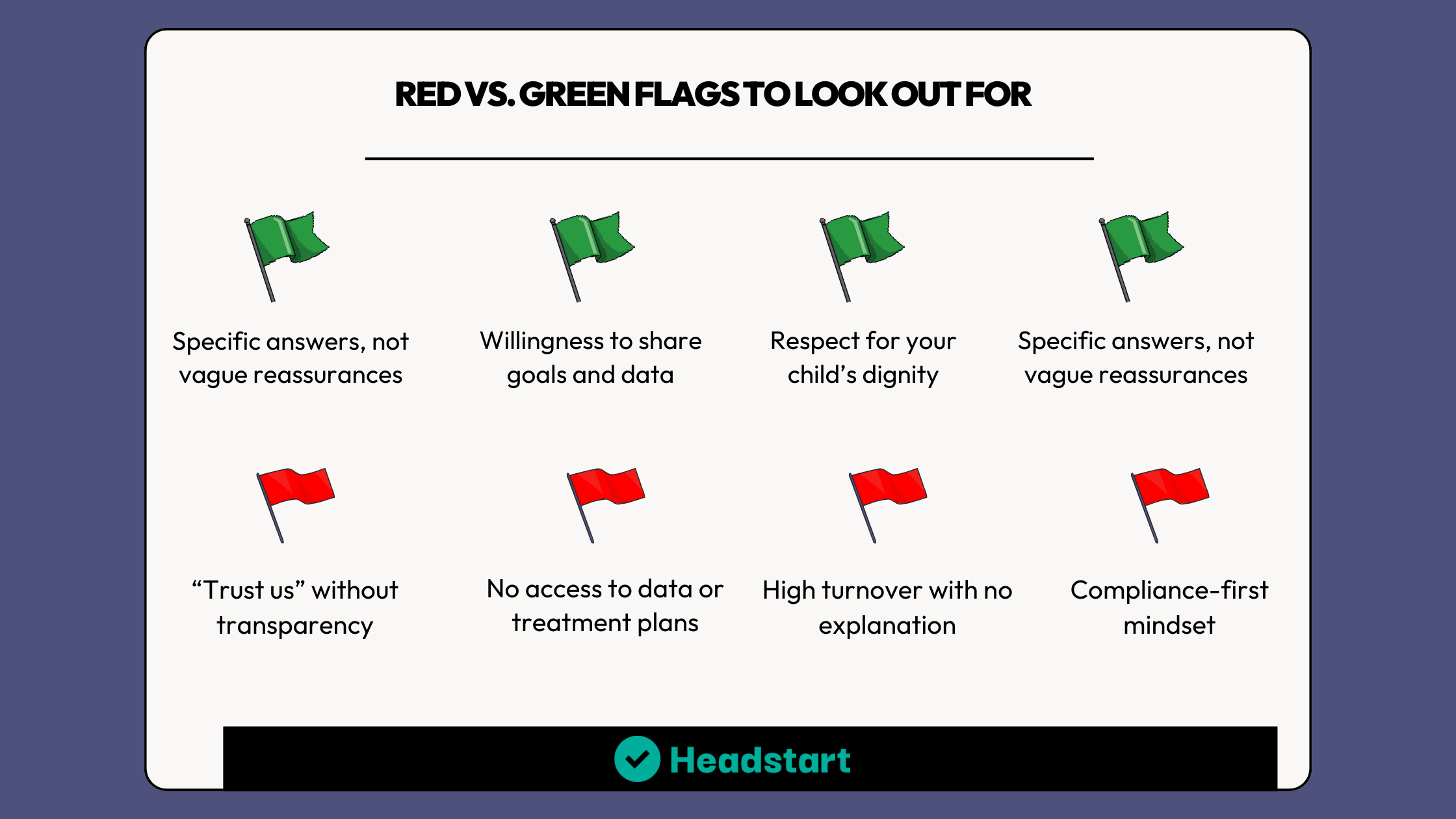
Red flag: You cannot get a straight answer about who is on your child’s case or how long they have been trained.
2. How often will the BCBA personally observe sessions and update the plan?
Your BCBA should not be a name on paper. They should be actively involved.
A strong answer sounds like:
Specific frequency (for example, weekly or biweekly)
Scheduled supervision and plan reviews
Willingness to include you in part of those observations
Red flag: Vague answers like “as needed” with no structure.
3. Can I see the treatment plan and goals in plain language?
You should always have access to your child’s goals and understand what they are working toward.\
A strong answer sounds like:
You receive a copy of the treatment plan
Goals are functional and meaningful to daily life
Willingness to explain why each goal matters
Red flag: Goals are hidden, overly technical, or never reviewed with you.
4. How did you decide how many hours my child needs?
More hours does not always mean better care. The right number of hours should be based on assessment and progress, not a default recommendation.
A strong answer sounds like:
Hours are tied to specific goals and needs
Ongoing review of whether hours should increase or decrease
A long-term plan for independence
Red flag: The same number of hours is recommended for every child.
5. How will you measure progress, and how often will I see the data?
If progress is happening, it should be visible.
A strong answer sounds like:
Clear explanation of how skills are measured
Regular data reviews shared with parents
Honest conversations when progress slows
Red flag: You are told to just trust the process without seeing evidence.
6. What does a great session look like, and what happens if my child is upest?
Therapy should build skills, communication, and confidence, not just compliance.
A strong answer sounds like:
Teaching through motivation and reinforcement
Plans for breaks, regulation, and communication
Respect for your child’s signals
Red flag: Pushing through distress without a plan.
7. How do you protect my child’s dignity, individuality and voice?
Your child is not a checklist. They are a person.
A strong answer sounds like:
Choice and preference built into sessions
Goals that improve quality of life
Respect for communication in all forms
Red flag: Focus on making a child look typical instead of helping them function and feel safe.
8. What strategies do you use, and what strategies will you not use?
You have a right to know what methods are being used.
A strong answer sounds like:
Clear explanation of teaching strategies
Transparency about what is not used
Willingness to answer questions openly
Red flag: Secrecy or defensiveness around methods.
9. How will you involve me, and what will you teach me to do at home?
You are the constant in your child’s life.
A strong answer sounds like:
Practical parent training
Support that fits your real life
Collaboration without blame
Red flag: Parent involvement is treated as optional or guilt-driven.
10. How do you coordinate with school, speech, OT, and other providers?
Your child does not live in a silo.
A strong answer sounds like:
Willingness to collaborate with consent
Consistent goals across settings
Clear communication channels
Red flag: No coordination or unwillingness to collaborate.
If there’s one thing to remember, it’s this: asking questions does not make you difficult. It makes you informed, involved, and protective of your child’s care. The right ABA provider will welcome your questions, not dodge them. They will see you as a partner, not a problem. You deserve clarity, transparency, and confidence at every step of this process. To make these conversations easier, we created a simple, printable question guide you can bring to intake meetings, check-ins, or progress reviews.
Download the one-page question guide below and walk into your next conversation prepared, empowered, and supported.